Breast cancer – unfortunately common
Currently, breast cancer is the most common type of cancer in Germany. According to a survey by the Robert Koch Institute (RKI), about 3 out of 10 women experience breast cancer. Treatment by chemotherapy or surgery is often combined with adjuvant radiation therapy.
approx. 30 %
of new cancer cases in women are breast cancer
approx. 88 %
relative survival rate after five years
Source: “Cancer in Germany”, RKI/Krebsdaten.de
Where can you get breast cancer treatment in Munich?
Breast cancer(mammary carcinoma) is the most commonly diagnosed cancer in women. If this type of cancer is detected during an examination, it is important to jointly develop an individually tailored treatment plan to efficiently treat the tumor.

How is breast cancer treated?
It is crucial to correctly classify the tumor stage (UICC) and to know the possible spread of cancer cells in the body (TNM system) in order to develop the treatment plan. Nowadays it is standard that cancer cells are analyzed with respect to special characteristics (e.g. hormone receptor status, Ki67, Her2neu receptor and others).
The so-called Oncotype test can help decide whether chemotherapy is appropriate or not. On the basis of the information then available and taking into account the patient’s personal wishes and life situation, the attending physician decides with the patient whether surgery, chemotherapy, radiotherapy or hormone therapy is suitable and sensible.
Radiotherapy
Adjuvant radiotherapy is useful to reduce the risk of recurrence after surgery. If metastases are present, they can be treated specifically, e.g. to relieve pain or to increase stability at the bone. Radiation therapy may also be used as a primary treatment modality in rare cases when surgery is not an option. This is the case, for example, if certain pre-existing conditions do not allow surgery or if the patient refuses surgery.
Breast cancer is irradiated with high-energy radiation percutaneously – that is, through the skin from the outside. In so-called teletherapy, the radiation concentration is directed selectively at the cancerous region in order to spare healthy surrounding tissue as much as possible. In addition, internal radiation(brachytherapy) may be used in some circumstances. The aim of both methods is to stop cell growth in order to prevent spreading in the body.
Operation
With few exceptions, surgery is one of the most important elements of breast cancer treatment. Surgeons perform breast-conserving surgery whenever possible. This is the case when the tumor is localized and can be completely removed.
Removal of the breast (mastectomy), on the other hand, is necessary when the tumor is already larger, has spread, cannot be completely removed in any other way, or radiation therapy is not possible. Lymph nodes may also need to be removed if cancer cells are detectable in them.
Chemotherapy
Chemotherapy can be used either before (neoadjuvant) or after surgery (adjuvant). Used before surgery, it can shrink the breast tumor. After surgery, chemotherapy can help reduce the risk of recurrence by reducing regrowth or the possible spread of cancer cells in the body.
Hormone therapy
Hormone therapy aims to stop cancer growth. Cancer cells – just like healthy mammary gland cells – have receptors to which female hormones (estrogen and progesterone) can dock and promote growth. If these receptors are blocked by hormone therapy, the female hormones cannot dock – thus growth is prevented.
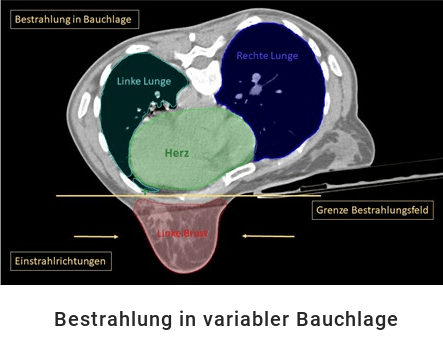
Breast cancer irradiation in prone position
Radiation for breast cancer can affect adjacent organs, such as the heart and lungs. For this reason, therapy is now often performed in the prone position.
Our radiation therapy sites have gone one step further and offer prone radiation with variable positioning. The position board is not fixed as usual, but can be tilted up to 10 degrees in the longitudinal axis. Without compromising the patient’s bearing safety and significantly improving the irradiation area, the burden on healthy tissue decreases considerably.
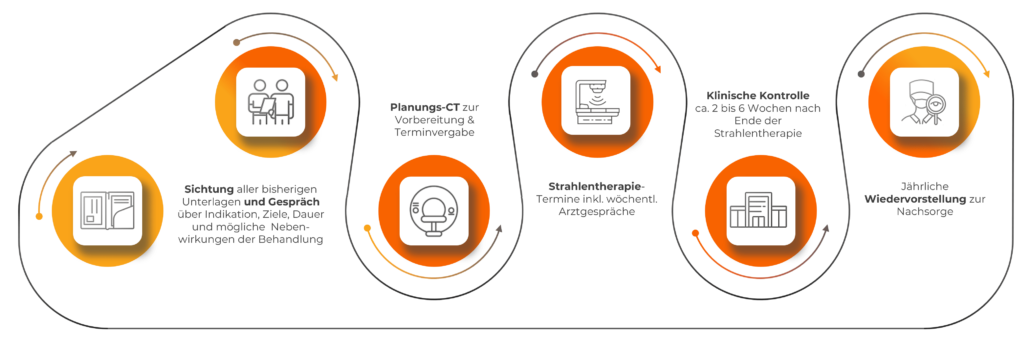
What is the treatment process in our practices?
What do you need to know before the treatment?
Please make sure you eat a healthy, balanced diet and drink enough water. A healthy nutritional status plays an important role in the treatment and spread of the tumor, it also helps reduce the side effects of therapy. Alcohol and smoking should be avoided.
During and after treatment
After breast cancer treatment, follow-up is elementary to make sure that the patient is doing well, that the treatment was successful, that there were no subsequent complications and that there was no recurrence. Your gynecologist usually performs a follow-up examination every three months, which includes, for example, a palpation and an ultrasound. With the help of a mammogram – usually carried out every 6 months after therapy – the glandular tissue can be additionally examined and assessed.
Most of the complaints recede with time and can also disappear completely. Every now and then you may feel a little tired from the radiation, this is also called “radiation hangover”. This fatigue also goes away after the end of the therapy. Sometimes the lymphatic channels must also be treated. In such a case, there may be a slight scratching in the throat at the end of the therapy, which will subside after the end of the therapy. Patients are seen by a doctor during therapy and, depending on the symptoms, appropriate creams or medications are prescribed, which usually quickly alleviate the symptoms.
What are the side effects of breast cancer treatment?
The treatment plan is individually tailored to the patient so that the cancer can be treated in the best possible way. Although the therapy should not be unduly stressful for the patient, side effects can still occur during and after the individual treatment steps.
Radiation therapy is usually very well tolerated by patients. In contrast to chemotherapy, this is a local and not a systemic therapy, so that the side effects to be expected usually also occur only locally. This can be, for example, a reddening of the skin in the irradiated area – comparable to a sunburn. This usually occurs after the third week of treatment. In the further course, the skin then turns brown – as we also know from a sunburn – and then returns to the initial state before the start of radiation therapy.