Prostate cancer – good therapy options
In prostate cancer, severe tumor stages have become significantly rarer. The reason for this is the good prostate cancer early detection . The relative survival rate is about 89 percent – very high compared to other types of cancer (surveys by the Robert Koch Institute).
1 from 5
of new cancer cases in men involve the prostate gland
approx. 89 %
relative survival rate after five years
approx. 50 %
Decline in mortality rate in the last 20 years
Source: “Cancer in Germany”, RKI/Krebsdaten.de
Where can you have prostate cancer treated in Munich?
Prostate cancer(prostate carcinoma) is the most commonly diagnosed cancer in men. If the tumour is detected during an examination, the doctor chooses an individual therapy plan in consultation with the respective patient in order to treat the cancer successfully.
The team of Radiologie München supports colleagues from other disciplines in the development of an individual treatment plan within the framework of tumour boards in order to ensure the best possible therapy.
What is a tumor board?
Tumour boards are conferences in which specialists from different fields discuss the respective case together. In doing so, they jointly determine the optimal strategies for diagnostics and therapy.

How is prostate cancer treated?
The treatment of prostate cancer depends primarily on how advanced the cancer is, whether it is localized or whether metastases have already been detected in other organs. In a very early, localised and non-aggressive stage, it may be sufficient to actively monitor the cancer (Active Surveillance) or to observe it in the long term (Watchful Waiting), as symptoms only appear after some time. If changes are detected, a decision should be made about suitable therapy in consultation with the doctor.
At a more aggressive or advanced stage, when the cancer is no longer localized, surgery or radiation therapy is necessary. Depending on the situation, hormone therapy and/or chemotherapy may also be recommended.
Radiotherapy
Radiation therapy may be used after surgery to reduce the risk of recurrence (adjuvant radiation). Similarly, radiotherapy is used when there is a rise in PSA (salvage radiotherapy) or when PSA levels do not drop completely after surgery (additive radiotherapy). If the PSA level rises or does not fall sufficiently, a PSMA PET/CT scan is now often sought to detect the cells that form the protein PSA.
Radiation therapy is an equivalent alternative to surgery in an early and an advanced stage (without metastases)(definitive radiation therapy). In certain situation, radiotherapy is combined with anti-hormonal therapy (tablets or depot injections) for a certain period of time. If metastases have already been detected, high-dose palliative radiotherapy can help prolong life and prevent prostate-specific symptoms prophylactically.
Teletherapy – percutaneous irradiation at any stage
Percutaneous radiotherapy (teletherapy) can be used at any stage of prostate cancer. In this procedure, the prostate is irradiated with a high-energy dose of radiation from various directions from the outside through the skin. The irradiation field is precisely adjusted to protect the surrounding healthy tissue.
Brachytherapy – the other method of irradiation of prostate cancer
In brachytherapy, the radiation source (radionuclide) is introduced into the prostate. A distinction is made between LDR and HDR brachytherapy. In LDR brachytherapy , low-dose (“low-dose rate”) radiation pens are placed in the prostate and left there until their radioactive effect has worn off. HDR brachytherapy uses a much higher dose (“high-dose rate”) radiation source. The radionuclides are removed after a short time.
Which method is used depends on the patient’s risk profile. In the case of a localized tumor, all the forms of radiotherapy described can be used. Percutaneous radiotherapy and HDR brachytherapy are used for locally advanced findings.
Operation
If the cancer is confined to the prostate, the prostate and adjacent tissue, and in some cases the lymph nodes, are surgically removed. Therefore, surgery may be useful up to an advanced stage.
Hormone therapy
Hormone therapy is used to support primary treatment and when the cancer has spread and metastasized to lymph nodes or bone. Here, drugs are used that spread their effects throughout the body. In this way, the spreading cancer cells are attacked. The goal of this method is to slow or stop the spread of cancer cells to other organs. In addition, hormone therapy relieves pain caused by metastases.
Chemotherapy
In an advanced, metastatic stage of cancer, chemotherapy may be used concomitantly. The drugs used (cytostatics) slow or stop the spread of cancer cells in the body by disrupting the growth of the malignant cells. This alleviates discomfort caused by illness.
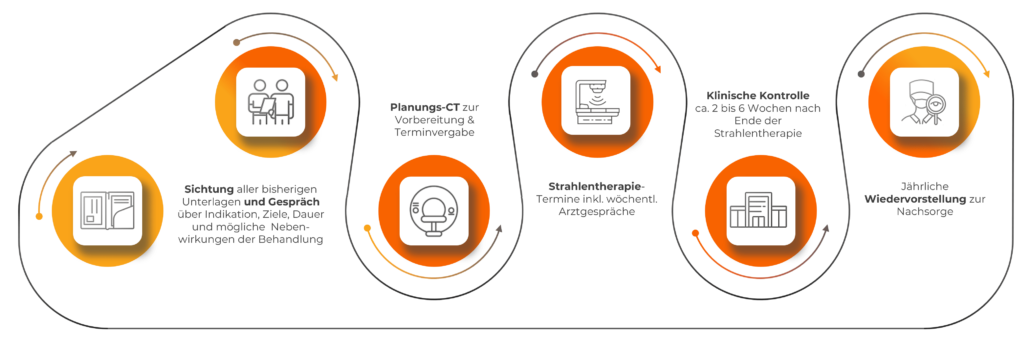
What is the treatment process in our practices?
What do you need to pay attention to before, during and after treatment?
Please make sure you eat a healthy, balanced diet and drink enough water. A healthy nutritional status plays an important role in the treatment and spread of the tumor, it also helps reduce the side effects of therapy. Alcohol and smoking should be avoided.
Individual treatment methods against prostate cancer can affect the patient’s quality of life because the treatment is exhausting. Please inform your attending physician about your side effects. Adjusting the medication composition or dosage may provide relief.
Stay active! On the one hand, exercise and muscle training have a positive influence on cancer treatment and its consequences, as the patient can tolerate them better. On the other hand, physical exercise lowers the risk of relapse.
What are the side effects of treatment of the prostate?
The treatment of prostate cancer is individually tailored to the patient so that the therapy has the greatest chance of cure while sparing the patient as much as possible. Nevertheless, side effects may occur according to the severity of the disease and treatment measures. Erectile dysfunction and bladder weakness are often noted because prostate function has been compromised.
Some treatments are burdensome for the body. Feelings of weakness, pain, muscle or bone loss, or weight gain may occur. Mucosal inflammation in the urinary bladder, stomach and digestive tract, and hair loss may also occur. Hormone or chemotherapy may affect the immune system.